It was a night like any other. Celline Bautista and her husband Jacob were at home with their three-year-old daughter Noelle and preemie baby Noah. Celline had just breastfed Noah, and they were about to burp him when Jacob sensed that something was wrong.
Noah had gone pale. His lips turned gray, his eyes rolled out, and his arms fell to his side.
Celline recalls, “His color was changing. He wasn’t responding. He was just out. Everyone at home just started crying.”
The situation was alarming, to say the least. One moment Noah was fine, and the next, it was like the life was slowly draining out of him!
What was happening?!
WAY TOO EARLY
Celline had a relatively smooth sailing pregnancy, but started getting really busy around Christmas.
“We moved houses. I had an assistant that resigned from the store, so I took her work. I had weddings. I had to go to Tagaytay. I had to go to Baguio. Tagtag talaga. I was eight months pregnant and I was working on one of my bestfriend’s wedding. I don’t get tired easily. But I was planning to slow down mid-February,” she recalls.
Celline went to a wedding in Tagaytay on January 14. A couple of days later, on January 18, she had some spotting. “It was just drops,” she says.
Nevertheless, the couple immediately went to the hospital, where the doctors advised her to go on bed rest at home. The next day, however, Celline found herself contracting. Because she has a high tolerance for pain, she didn’t think it was a big deal.
But the contractions continued, and on the morning of January 20, Celline and Jacob went to the hospital once again. Celline didn’t know it but she was already 4 cm dilated.
The doctors immediately went to work. It was way too early for Celline to give birth. She was only 32 weeks along.
She recalls, “They put me in the ICU because I had to be given magnesium sulfate which stops you from contracting. It’s the most painful thing in the universe.”
Celline was also given steroids. Administering steroids on the mother can help her unborn baby’s lungs to develop more quickly.
But by 6:30 PM, Celline recalls feeling her whole body being pulled down. When her doctors checked, she was already 7 cm dilated. It was the point of no return. She was prepped for a C-Section, and before midnight, she had given birth to baby boy Noah. Because of his frail state though, Noah was immediately whisked to the Neonatal Intensive Care Unit (NICU).
She recalls, “I saw Noah very briefly. They gave him to me but they never put him on my breast. They just took one photo. He never latched.”
The next day, Celline visited Noah in the NICU.
“Seeing him for the first time was a nightmare,” she says.
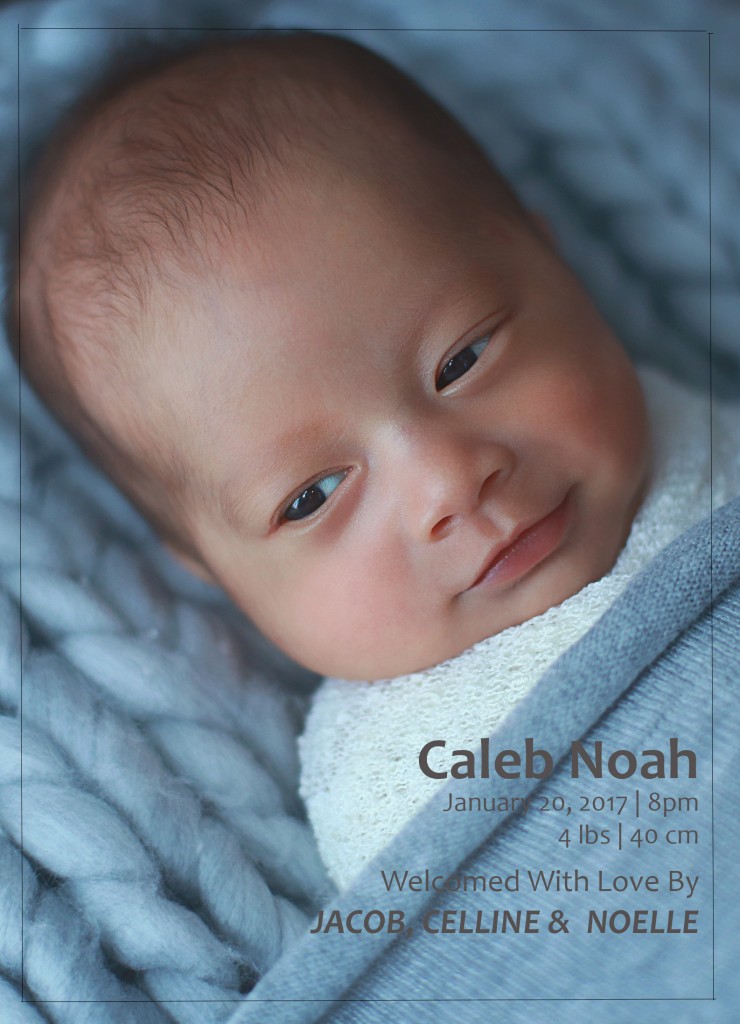
“He was intubated. He was on a ventilator. He was on antibiotics. But he wasn’t really very small. He was 4 pounds.”
But every day, Noah became stronger and stronger. Every day, there was progress. The tubes were removed. He started sucking.
“There was always a new thing. He was getting better,” says Celline.
And on his 15th day, Noah was finally able to go home.
One of the hospital’s requirements before Noah was discharged was for Jacob and Celline to learn how to do cardiopulmonary resuscitation (CPR). Celline explains, “They would teach you how to do CPR because sometimes preemie babies forget to breathe. It’s called apnea. But Noah had no episode of apnea in the NICU.”
At home, things went swimmingly, and Noah just got stronger and stronger.
On the morning of March 2, the family went to Noah’s eye doctor. Because he was a preemie baby, there was a chance that his eyes may not have developed properly. On examination, however, his eyes were okay, giving much joy to his parents. They then took Noah to his pediatrician for his six-in-one shot.

THE NIGHT OF MARCH 2
When Noah turned gray on the night of March 2, his father immediately took action.
In his Facebook page, Jacob described the heart-thumping events of the next few moments:
“At this point I was at the brink of panicking but God gave me just enough courage to be strong for my girls. I tried saying Noah’s name aloud to rouse his consciousness, but still to no avail. Somehow, amidst all the hysteria I still remembered how to try to revive a baby when he isn’t breathing. I laid him on his back, tilted his head back, checked his mouth for any blockages, then administered CPR on him covering his mouth and his nose. Then I started pumping his chest with my fingers but all I got was a small squeaking sound from our Noah.”
“Celline, who at this point was talking to Noah’s pediatrician on the phone, urged us to rush him to the hospital. So we quickly picked up the car keys and ran to the elevator of our condo. Even here, while carrying Noah, I was trying to pump his chest hoping that he would be revived. I asked Celline to blow air into him this time since I couldn’t do it while carrying him. I repeated to pump his chest again while Celline was blowing through his mouth and nose.”
“Finally, just as we reached the ground floor, our fighter Noah gasped for as much air as he could before then crying his lungs out. We finally revived him after about three to four of the longest minutes I imagine a parent could ever go through.”
Celline adds, “I remember that the elevator kept stopping on different floors. There was another guy on the elevator, and he was saying, ‘Emergency! Emergency!’ Before we hit the ground floor, Noah gasped for air. He started turning into his color and I super cried. We got in the car, and we were just honking at all the cars. When we got to the intersection, we couldn’t turn left. We begged the MMDA officer to let us pass. When he realized it was an emergency, he let us go. He even stopped traffic to let us pass, so we were in the hospital in two minutes.”
WHAT HAPPENED TO BABY NOAH?
Noah was admitted to the hospital for a series of tests. Celline and Jacob wanted to know what happened and why it happened. The first speculation was that Noah may have aspirated. But because no milk was found in his lungs, this conjecture was ruled out.
The second hypothesis was that the vaccine may have caused the episode. Celline was told that there was a one in a million chance that the vaccine may have such an effect on a person. But then again, there was really no way of knowing for sure whether it was the cause or not.
The third hypothesis was that Noah was suffering from an infection. But results of his blood culture were negative, so this was also ruled out.
Though Celline and Jacob may never know what really caused the episode, there is one thing that they are sure of: They are very grateful that they know how to administer CPR.
Celline advises parents: “You need to learn CPR. You take it for granted, all of these things. But there’s really a reason for everything. Don’t be lazy. To be honest, when they first told us that we had to go through it, I thought, ‘Do we really need it?’ But I believe there is a reason for everything. God has a reason.”
In his Facebook post, Jacob shares the same advice.
“Knowledge can spell the difference between life and grave danger… So if you have a newborn baby (especially premature), infant, or even toddler, I strongly encourage you to ask your doctor or the head nurse how to administer CPR or attend a baby saving class which will only take about half an hour of your time. That’s the best class you could ever attend as a parent if you ask me. Be attentive, remember the minor details, as I also forgot one important thing, which is to rub his back to try to get some responsiveness from our baby. Ask relevant questions like how much pressure to pump, how much air to blow, etc. We were fortunate to know what to do because our baby was born premature and considered high risk. That’s why our nurse taught us. But I don’t recall them giving us this lesson when our first child (full term baby) was born. So I strongly recommend knowing how to do this properly. We still have our baby in our arms because of this simple knowledge.”
Check this link to know how to perform CPR.


Leave a Reply